In the world of modern medicine, hysteroscopy is an excellent demonstration of innovation and precision. Hysteroscopy is a minimally invasive surgical procedure that allows doctors to scan the inside of a woman’s uterus through a hysteroscope, a thin tube attached with a small camera and light.
Since its discovery in 1869, hysteroscopy has truly revolutionized the field of gynecology. Today it has helped millions treat various gynecological disorders and is only expected to rise in prevalence.
In this blog, we will dive deep into understanding hysteroscopy, its types, procedures, recovery, and more. If you’re considering hysteroscopy or just curious about it, this is an excellent read for you.
Defining Hysteroscopy
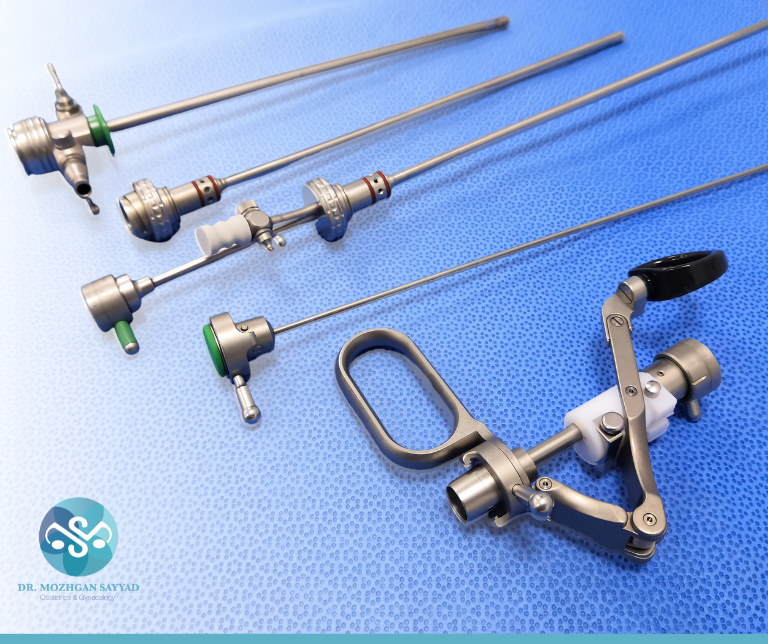
Hysteroscopy is a medical procedure that scans the inside of the uterus by inserting a hysteroscope through the cervix. A hysteroscope is a slender tube that’s attached to a light and camera to allow surgeons to examine the uterus cavity in real-time. Hysteroscopy is a versatile tool in gynecology as it can be used for diagnostic and therapeutic purposes.
Types of Hysteroscopy
The five different types of hysteroscopy are:
- Diagnostic Hysteroscopy: Diagnostic hysteroscopy is a procedure where the fundamental goal is to detect any structural abnormalities or irregularities in the uterine cavity that may be causing unusual bleeding. Additionally, it is also used to verify the results of other tests, like an ultrasound or HSG.
- Operative Hysteroscopy: In operative hysteroscopy, not only does the doctor evaluate the uterine cavity, but they also treat it simultaneously. Some of the common treatments include: [I] Polypectomy [Removal of Uterine Polyps], [ii] Myomectomy [Removal of Small to Medium-Sized Uterine Fibroids], [iii] Adhesiolysis [Separation of Uterine Adhesions or Scars], [iv] Endometrial Ablation [Destruction or Removal of Uterine Lining], and [v] Uterine Septum Resection [Correction of Uterine Septum].
The treatment is done through electric current, freezing, heat, or chemicals. - Hysteroscopic Sterilization: Hysteroscopic sterilization is an operative hysteroscopy that’s used for permanent contraception. During the procedure, a small device is inserted into the fallopian tubes to create scar tissues that block the tubes.
- Office-Based Hysteroscopy: Office-based hysteroscopy is a minimally invasive procedure that’s primarily for diagnostic purposes or treating minor conditions. As the name suggests, this type of hysteroscopy is done in the doctor’s office and does not require anesthesia, making it a convenient procedure for patients. Office-based hysteroscopy is used to diagnose and treat abnormal uterine bleeding, infertility, and recurrent pregnancy loss.
- Flexible Hysteroscopy: Flexible hysteroscopy uses a thinner and highly flexible hysteroscope with a wide 100-degree angulation for diagnosis and minor procedures. It’s extremely useful when there is limited access or in tight cervical conditions. Undoubtedly, its significant benefit is that it can observe the entire uterine cavity.
Every type of hysteroscopy has its own advantages and is selected according to the patient’s condition and needs. Some of the factors that influence the selection of hysteroscopy include the purpose of the procedure, the patient’s medical history, and the doctor’s expertise.
Purpose
The primary purpose of hysteroscopy is to examine the uterus and diagnose/treat gynecological issues. Additionally, your doctor may recommend hysteroscopy for the following reasons:
- To investigate symptoms like heavy bleeding, abnormal vaginal bleeding, postmenopausal bleeding, pelvic pain, recurrent miscarriages, or difficulty getting pregnant.
- To diagnose and treat the causes of abnormal uterine bleeding.
- To verify results from other tests like an ultrasound and HSG.
- To remove abnormal growths like polyps or fibroid tumors.
- To prevent bleeding by destroying tissues.
- To diagnose and treat conditions through a single non-invasive surgery.
- To locate abnormalities and treat them without damaging the neighboring tissues.
- To perform hysteroscopic sterilization for permanent contraception.
- To manage and monitor conditions that affect the uterus.

Candidate for Hysteroscopy
Some of the factors that make you a candidate for hysteroscopy are:
- Abnormal Uterine Bleeding
- Abnormal Growth [Polyps, Fibroid Tumors]
- Abnormal Pap Smear Results
- Infertility or Recurring Miscarriages
- Difficulty in Conceiving
- Chronic Pelvic Pain
- Unexplained Pelvic Mass
- To Monitor Medical Conditions
- To Evaluate Uterine Abnormalities
- To Evaluate Abnormal Imaging Findings

However, hysteroscopy is not recommended if you:
- Are pregnant
- Suffer from pelvic infection
- Suffer from medical conditions that make anesthesia or surgery risky
- Have anatomical abnormalities that make hysteroscopy difficult or impossible
Procedure
The general procedure of hysteroscopy is as follows:
- Preparation
- Your doctor will review your medical history, medications, and allergies.
- They will inform you of the procedure, including its purpose, benefits, and potential risks.
- Before hysteroscopy, you may be asked to fast for a certain period, especially if they use general anesthesia.
- Anesthesia
- Depending upon your condition and type of hysteroscopy, you may receive one of the following types: [I] Local Anesthesia [Numbing of the Cervix and Uterine Lining], [ii] Conscious Anesthesia [Mild Anesthesia to Manage Discomfort and Help Relax] [iii] General Anesthesia [Completely Numbed Throughout the Procedure]
3. Cervical Preparation
- After positioning you on the examination table with your feet raised [similar to a pelvic exam], your doctor will gently clean the vaginal and cervical area.
4. Visualization
- Once the hysteroscope is inserted, your doctor will scan the uterine cavity for abnormalities. They also introduce a clear, usually saline, solution into the uterus to expand it and get a better understanding.
5. Examination & Treatment [If Necessary]
- Your doctor will examine the uterine lining and may take images/videos if the procedure is diagnostic. However, if any issues are detected, the doctor can perform therapeutic procedures like removal of uterine polyps, correction of uterine septum, removal of fibroids, etc.
6. Completion & Recovery
- Once the procedure is complete, you may be kept under observation for a brief period, especially if you were sedated or provided general anesthesia.
- Most patients can return home on the same day. It’s recommended to arrange for someone to drive you home, especially if you received sedation or general anesthesia.
7. Aftercare
- After a hysteroscopy, it’s normal to experience mild cramping, spotting, or vaginal discharge for a day or two.
- Your doctor will also provide you with post-procedure care, which you must follow.
Ultimately, hysteroscopy is a generally safe and non-invasive procedure that has a short recovery time.


Benefits of Hysteroscopy
Some of the key benefits of hysteroscopy are:
- It provides accurate diagnosis
- It is a minimally invasive procedure
- It offers targeted treatment
- It enhances fertility by addressing uterine abnormalities
- It reduces uncomfortable menstrual symptoms
- It offers quick recovery
- It is an outpatient procedure where the patient can go home on the same day
- It has high success rates, with an overall 73% success in treating and managing abnormal uterine bleeding, infertility, abortion, etc.
- It has minimal scarring effects
- It improves the overall quality of life
It’s important to note that the benefits of hysteroscopy are largely based on your specific symptoms, and your doctor can recommend the right procedure for you.
Potential Risks
As with all procedures, hysteroscopy also comes with its potential side effects. Some of it are:
- Cramping
- Scarring
- Infection
- Fluid Overload
- Heavy Bleeding
- Pelvic Inflammatory Disease
- Complications from fluid/gas used to expand uterus
- Complications from anesthesia
- Puncture of the uterus or cervix
- Tearing of the uterus [rare] or damage to the cervix
It’s important to state that the risks of hysteroscopy are generally low, and most patients experience no side effects.
Alternatives to Hysteroscopy
There are several alternatives to hysteroscopy, and the choice of alternative will depend on individual conditions, preferences, and the doctor’s recommendation. Some of the common alternatives are:
- Ultrasound
- MRI Scan
- CT Scan
- Endometrial Biopsy
- HSG
- Laparoscopy
- Dilation and Curettage [D&C]
- Biopsy Using a Small Tube
- Anti-Inflammatory Medications
- Medical Management
- Watch-and-Wait Approach
Get Help with Dr. Mozhgan
As you can see, hysteroscopy is an excellent method for diagnostic purposes and minimal procedures. If you’re in search of a qualified professional to perform hysteroscopy, consider Dr. Mozhgan. She is a highly experienced gynecologist with over 20 years of knowledge and practice. Dr. Mozhgan guarantees to offer you personalized care and treatment to help you achieve your best life.
Take control of your health today!
FAQs
Q1. What symptoms should I look out for after hysteroscopy?
Contact your doctor immediately if you experience the following symptoms:
- Fever
- Severe Abdominal Pain
- Heavy Vaginal Bleeding
Q2. Should I be worried about undergoing a hysteroscopy?
Absolutely not. Hysteroscopy is a non-invasive procedure with limited risks!
Q3. How painful is hysteroscopy?
The level of pain experienced during a hysteroscopy can vary from individual, based on several factors like pain tolerance, type of hysteroscopy, and whether anesthesia/sedation is used.
Q4. What happens to my uterus after a hysteroscopy?
After a hysteroscopy, the uterus usually undergoes a process of recovery and healing. The specific effect on the uterus is largely influenced by whether the procedure was diagnostic or included targeted treatment. It’s common to experience bleeding that lasts longer if hysteroscopy was used for treatment. Moreover, if the doctor fills the uterus with air, your belly may feel full.
Q5. What is the difference between hysteroscopy and D&C?
Hysteroscopy is a diagnostic and operative procedure that allows your doctor to scan, diagnose, and treat the uterus cavity for various gynecological issues. On the contrary, D&C is a surgical procedure that dilates the cervix and scraps the lining of the uterus to diagnose or treat abnormal uterine bleeding. While both target the uterus, the purpose and types of anesthesia used vary.