Colporrhaphy is a minimally invasive surgical procedure aimed at correcting pelvic organ prolapse, anterior prolapse, and posterior prolapse. There are mainly two types of colporrhaphy, anterior colporrhaphy [which corrects anterior prolapse] and posterior colporrhaphy [which corrects posterior prolapse]. The normal recovery period for the surgery is three months.
What is Colporrhaphy?
Colporrhaphy is a minimally invasive surgical procedure aimed at correcting, repairing, or reinforcing the walls of the vagina and treating pelvic organ prolapse. The primary aim of colporrhaphy is to address conditions like pelvic organ prolapse and restore its condition back to normal.
Related: Pelvic Organ Prolapse | Vaginal Repair Surgeries
Types of Colporrhaphy
There are several types of colporrhaphy that are dedicated to correcting specific issues of the vagina. However, the most common ones are:
- Anterior Colporrhaphy: Anterior colporrhaphy is a surgical procedure that corrects abnormalities in the front [anterior] wall of the vagina. It is typically performed to address cystocele, a condition where the bladder protrudes into the vagina.
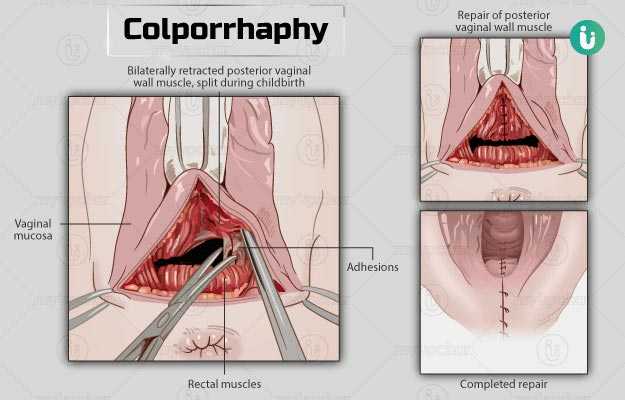
- Posterior Colporrhaphy: Posterior colporrhaphy is a surgical procedure that corrects abnormalities in the back [posterior] wall of the vagina. It is typically performed to address rectocele, a condition where the rectum bulges into the vagina.

Understanding Anterior and Posterior Prolapse
Causes of Anterior and Posterior Prolapse
Anterior and posterior prolapse can occur due to a variety of reasons. Some of the common causes are:
- Pregnancy or Childbirth
- Aging
- Obesity
- Chronic Straining
- Hysterectomy
Symptoms of Anterior and Posterior Prolapse
Anterior and posterior prolapse can cause a variety of symptoms including:
- Vaginal or pelvic fullness
- A feeling of organs protruding out
- A bulge into the vagina canal or through the vaginal opening
- Difficult bowel movements
- Urinary incontinence
- Lower back pain
- Discomfort during intercourse
- Difficulty in peeing or the feeling of incomplete pee

Understanding Pelvic Organ Prolapse
Pelvic Organ Prolapse, Causes & Symptoms
Pelvic organ prolapse or POP is a condition where the muscles and ligaments supporting a woman’s pelvis weaken due to childbirth, hysterectomy, or menopause. It causes the pelvic organs [vagina, cervix, uterus, bladder, urethra, and rectum] to drop low, creating a bulge in the vagina.
Symptoms of pelvic organ prolapse include a sensation of pressure in the pelvic region, continuous discomfort on the vagina, a feeling of something coming down on the vagina, and difficulty in peeing or passing stool.
Benefits of Colporrhaphy
Colporrhaphy offers tremendous benefits. Some of them are:
- Symptom Relief: As expected, the fundamental benefit of undergoing colporrhaphy is that it relieves the uncomfortable symptoms of pelvic organ prolapse, anterior prolapse, and posterior prolapse.
- Restoration of Pelvic Organ Position: As the surgery corrects pelvic abnormalities, the organs will be repositioned into the right place.
- Minimally Invasive: Unlike traditional surgeries, colporrhaphy is a minimally invasive surgery that offers fast recovery and low postoperative discomfort.
- Enhanced Sexual Experience: As colporrhaphy relieves the uncomfortable symptoms of prolapse, it has been shown to improve sexual satisfaction.
- Improved Quality of Life: Lastly, colporrhaphy alleviates the discomfort associated with prolapse, thus improving the overall quality of life.

Risks or Side Effects of Colporrhaphy
As with any surgical procedure, colporrhaphy also comes with its set of side effects. Some of the common risks are as follows:
- Infection: There is always a risk of infection with any surgical procedure, including colporrhaphy.
- Bleeding: Although some bleeding is common during the procedure, there is a chance of excessive bleeding during or after the surgery.
- Injury to Other Pelvic Region: There is a chance of injuring other pelvic structures like the bladder or rectum during the procedure.
- Urinary & Bowel Issues: Some patients may experience temporary difficulty while peeing or passing stools.
- Recurrent Prolapse: In some cases, there is a chance of recurring prolapse even after the surgery, especially if the underlying cause isn’t addressed.
- Mesh-Related Complications: If synthetic mesh is used in the surgery, there is a risk of infection, erosion, and pain.
- Anesthesia Complications: Although it’s rare, there is a chance of anesthesia complications.
- Dyspareunia: Some patients may experience uncomfortable or painful intercourse after the procedure.
- Scarring: Most scars from the procedure are internal, however, external scarring can occur.
Colporrhaphy – Procedure & Recovery
- What Happens Before Colporrhaphy
Some of the usual steps that happen before the procedure are:
- Consultation: The initial step of any surgery is to have a consultation with your doctor. You will discuss your symptoms, health status, and any other vital information that’s required.
- Evaluation: After the consultation, you will have a thorough evaluation of your medical status and symptoms to determine the need for colporrhaphy.
- Preoperative Instructions: You may receive preoperative instructions like fasting or discontinuing certain medications prior to the surgery.
- Anesthesia Discussion: The type of anesthesia used is also discussed with you before undergoing colporrhaphy.
- Postoperative Recovery: You may also be asked to arrange postoperative care like taking medical leave and arranging transportation back home during the initial recovery stage.
A2. What Happens During Colporrhaphy
The typical colporrhaphy procedure is as follows:
- Anesthesia: Depending upon your condition and your doctor’s recommendation, general, regional, or local anesthesia may be used.
- Incision: After administrating the anesthesia, an incision is made at the entrance of the vagina, extending towards the vaginal canal to access the weakened tissues.
- Repair of Prolapse: Once the weakened tissues are located, your doctor will repair and restructure them.
- Suturing: The incision is then sutured with strong and absorbable stitches to provide additional support to the pelvic organs.
- Anterior and Posterior Repair: Depending upon your condition, your doctor will perform either anterior or posterior colporrhaphy.
A3. What Happens After Colporrhaphy
After colporrhaphy, you may require a catheter, a tube inserted into the bladder to pass urine easily, for a few days. You will also be required to follow a liquid diet until you can continue your normal activities, which is typically for at least four weeks.
You will also have follow-up sessions with your doctor to track your progress and address any complications.
Get Help with Dr. Mozhgan
As you can see, colporrhaphy is a medical procedure that offers relief from prolapse symptoms. If you suffer from anterior, posterior, or pelvic organ prolapse, it’s important to seek medical attention. Contact Dr. Mozhgan, one of the best gynecologists in Dubai. With over 25 years of invaluable experience and knowledge, she is fully equipped to treat prolapse symptoms.
Book an appointment today & take control of your health!
Common FAQs
Q1. What are the alternatives to colporrhaphy?
Alternatives to colporrhaphy include non-surgical treatments like pelvic floor physical therapy, pessaries, vaginal repair with mesh, total colpoclesis, and InterStim therapy.
Q2. What is the recovery period for colporrhaphy?
The normal recovery period after the surgery is three months. During this period, you may be advised to:
- Take stool softeners
- Avoid straining during bowel movements
- Avoid lifting heavy objects [more than five pounds] and strenuous activities like weightlifting for at least six weeks after the surgery
- Avoid inserting tampons, vaginal douching, and intercourse for six to eight weeks after the surgery.


